When Your Child Has an Elbow Fracture
Your child has an elbow fracture. That means they have a crack or break in 1 or more of the bones of the elbow joint. The elbow joint is formed by 3 arm bones:
-
Radius. This is the bone on the thumb side of the forearm.
-
Ulna. This is the bone on the little-finger side of the forearm. The ulna forms the tip of the elbow.
-
Humerus. This is the upper arm bone that connects to the shoulder.
Your child may see a pediatric orthopedist for evaluation and treatment. An orthopedist is a healthcare provider who specializes in the diagnosis and treatment of bone and joint problems.
Types of fractures
Bones can break in many ways. Common types of fractures in children are:
-
Greenstick. This is when the bone bends, but it doesn’t break all the way through.
-
Nondisplaced. This is when the bone breaks completely, but the ends stay lined up.
-
Displaced. This is when pieces of broken bone don't line up.
-
Growth plate. This is a break near or through the growth plate. This is the soft part of a bone where the bone grows as the child grows. A growth plate injury can slow growth in that bone. Growth plate injuries may be difficult to treat.
Fractures when the broken bone comes through the skin are called open or compound fractures Fractures can also be referred to as closed when the broken bone does not come through the skin.
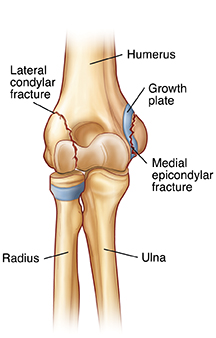 |
| Lateral condylar fracture and medial epicondylar fracture. |
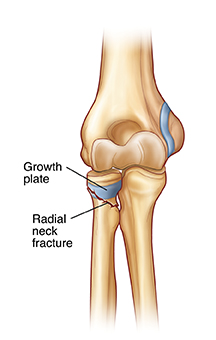 |
| Radial neck fracture. |
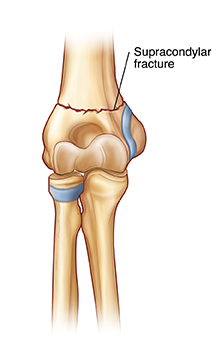 |
| Supracondylar fracture. |
What causes elbow fractures?
Elbow fractures often result from:
-
Falling on an outstretched hand
-
Falling directly on the elbow
-
Forcing the elbow joint to move in an unnatural way
-
Receiving a hard blow to the elbow
What are the symptoms of an elbow fracture?
-
Elbow swelling
-
Sudden intense pain in the elbow and forearm
-
Skin bruising or color change around the elbow
-
Elbow deformity
-
Stiffness, making the elbow hard to move
-
Numbness in the hand, a sign of potential nerve injury
How are elbow fractures diagnosed?
You may have brought your child to the emergency room for the initial treatment of the elbow fracture. A treatment plan must now be made to make sure the elbow heals correctly. The healthcare provider will ask about your child’s health history and examine your child. An imaging test, such as an X-ray, will be done. Imaging tests show areas inside the body, such as the bones. They give the provider more information about your child’s injury.
How are elbow fractures treated?
Your child’s treatment plan is determined by the type, location, and severity of the fracture. As instructed, your child should:
-
Ice the elbow 3 to 4 times a day for 15 to 20 minutes at a time. This can help relieve pain and swelling. To make a cold pack, put ice cubes in a plastic bag that seals at the top. Wrap the bag in a clean, thin towel or cloth. Never put ice or an ice pack directly on the skin. The cold pack can be put right on a cast or splint.
-
Wear a splint as instructed.
-
Wear a cast for 3 to 6 weeks.
-
Raise the arm to reduce swelling. Keep the elbow above heart level as often as possible.
-
Do physical therapy to restore range of motion once the cast or splint is removed.
Some fractures may need closed reduction (moving broken pieces of bone back into alignment). Closed reduction is done by manipulating the bones from outside of the body and needs no incisions. For fractures of the joint, of the growth plate, or severe fractures, surgery may be needed. During surgery, fixation devices (pins that go through the skin into the bone) may be put into a broken bone to hold it in place while it heals. These devices may need to be taken out by the healthcare provider about 3 to 6 weeks after surgery.
Call the healthcare provider or get medical care right away if your child has any of the following:
-
Fever (see “Fever and children” below)
-
Chills
-
Increasing pain
-
Tingling, numbness, or pain around the cast or splint
-
Increasing swelling around the injured area
-
Fingers that change color or feel cold
-
Severe itching under a cast (mild itching is normal)
-
A cast that feels too tight or too loose
-
Any drainage that comes through or out of the end of the cast
-
Blisters
-
Decreased ability to move fingers
-
A bad odor that comes from underneath the cast
Take your child to the emergency department if your child has trouble moving their fingers or thumb.
What are the long-term concerns?
Once your child’s cast is removed, their elbow may have:
-
Short-term (temporary) stiffness and some loss of motion. This is normal. The elbow should still work well.
-
Pain for 2 to 3 weeks, while the elbow continues to heal
-
A different look than before the injury
In severe cases, the nerves and arteries of the elbow can be injured. This can cause complications and make healing more difficult. Your child’s healthcare provider will give you more information.
Keep in mind
Healthcare providers are trained to recognize injuries like this one in young children as a sign of possible abuse. Several providers may ask questions about how your child was injured. Healthcare providers must, by law, ask you these questions. This is done to protect the child. Please try to be patient and not take offense.
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use the rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below are guidelines to know if your young child has a fever. Your child’s healthcare provider may give you different numbers for your child. Follow your provider’s specific instructions.
Fever readings for a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
Fever readings for a child age 3 months to 36 months (3 years):
-
Rectal, forehead, or ear: 102°F (38.9°C) or higher
-
Armpit: 101°F (38.3°C) or higher
Call the healthcare provider in these cases:
-
Repeated temperature of 104°F (40°C) or higher in a child of any age
-
Fever of 100.4° F (38° C) or higher in baby younger than 3 months
-
Fever that lasts more than 24 hours in a child under age 2
-
Fever that lasts for 3 days in a child age 2 or older